A Guide to Mastering Upper Extremity Manual Muscle Testing with a Handheld Dynamometer
 Manual Muscle Testing (MMT) with handheld dynamometers is a fundamental component of musculoskeletal assessment in rehabilitation settings. These portable devices provide objective measurements of muscle strength, aiding clinicians in evaluating and monitoring patients' progress accurately. In this article, we'll explore the specific techniques and instructions for performing manual muscle tests using handheld dynamometers for upper extremities.
Manual Muscle Testing (MMT) with handheld dynamometers is a fundamental component of musculoskeletal assessment in rehabilitation settings. These portable devices provide objective measurements of muscle strength, aiding clinicians in evaluating and monitoring patients' progress accurately. In this article, we'll explore the specific techniques and instructions for performing manual muscle tests using handheld dynamometers for upper extremities.
Shoulder Flexion
The primary muscle responsible for shoulder flexion is the anterior deltoid, located on the front of the shoulder. However, other muscles, including the clavicular portion of the pectoralis major and the coracobrachialis, also contribute to this movement to varying degrees.
Testing Procedure for Shoulder Flexion: Performing manual muscle testing for shoulder flexion involves several steps to ensure accuracy and reliability.
- Positioning: Position the patient comfortably in either a seated or standing position, with the arm relaxed at their side.
- Stabilization: Stabilize the scapula to isolate the movement to the shoulder joint. You can achieve this by gently pressing on the acromion process or by providing manual stabilization of the scapula with your non-testing hand.
- Palpation: Identify the insertion point of the anterior deltoid, which is typically located on the lateral aspect of the deltoid muscle, midway between the acromion process and the insertion of the deltoid onto the humerus.
- Testing: Instruct the patient to elevate their arm forward, raising it as high as possible in the sagittal plane (i.e., in front of the body).
- Application of Resistance: Place one hand on the distal forearm of the patient's testing arm to provide resistance. Apply pressure in the direction opposite to shoulder flexion, ensuring a gradual increase in resistance to assess the muscle's strength throughout the range of motion.
- Observation: Observe the patient's ability to maintain the position against resistance. Look for compensatory movements or substitutions, such as trunk leaning or scapular elevation, which may indicate weakness in the targeted muscle or muscles.
- Grading: Use a standardized grading scale, such as the Medical Research Council (MRC) scale or the Modified Oxford Scale, to assign a muscle grade based on the patient's performance. Grades typically range from 0 to 5, with 0 indicating no muscle contraction and 5 representing normal strength.
Shoulder Extension
The main muscle responsible for shoulder extension is the latissimus dorsi, a large muscle located on the back. Additionally, other muscles, including the teres major and posterior deltoid, contribute to this movement to varying degrees.
Testing Procedure for Shoulder Extension: Performing manual muscle testing for shoulder extension involves several key steps to ensure accuracy and reliability.
- Positioning: Position the patient comfortably in either a prone or standing position, with the arms resting by their sides.
- Stabilization: Stabilize the scapula to isolate the movement to the shoulder joint. You can achieve this by applying gentle pressure to the scapula or providing manual stabilization with your non-testing hand.
- Palpation: Identify the insertion point of the latissimus dorsi, which is typically located on the posterior aspect of the humerus, near the medial epicondyle.
- Testing: Instruct the patient to move their arm backward, extending it as far as possible behind their body.
- Application of Resistance: Place one hand on the distal forearm or wrist of the patient's testing arm to provide resistance. Apply pressure in the direction opposite to shoulder extension, ensuring a gradual increase in resistance to assess the muscle's strength throughout the range of motion.
- Observation: Observe the patient's ability to maintain the position against resistance. Look for compensatory movements or substitutions, such as trunk extension or scapular retraction, which may indicate weakness in the targeted muscle or muscles.
- Grading: Use a standardized grading scale, such as the Medical Research Council (MRC) scale or the Modified Oxford Scale, to assign a muscle grade based on the patient's performance. Grades typically range from 0 to 5, with 0 indicating no muscle contraction and 5 representing normal strength.
Shoulder Abduction
The deltoid is the primary muscle responsible for shoulder abduction. The deltoid consists of three distinct portions: the anterior deltoid, middle deltoid, and posterior deltoid. Additionally, other muscles, such as the supraspinatus, contribute to this movement and play a supporting role in shoulder stability.
Testing Procedure for Shoulder Abduction: Performing manual muscle testing for shoulder abduction involves several key steps to ensure accuracy and reliability.
- Positioning: Position the patient comfortably in either a seated or standing position, with the arms resting by their sides.
- Stabilization: Stabilize the scapula to isolate the movement to the shoulder joint. You can achieve this by applying gentle pressure to the scapula or providing manual stabilization with your non-testing hand.
- Palpation: Identify the insertion point of the deltoid, which is typically located on the lateral aspect of the humerus.
- Testing: Instruct the patient to lift their arm sideways away from their body, elevating it as high as possible in the coronal plane.
- Application of Resistance: Place one hand on the distal forearm or wrist of the patient's testing arm to provide resistance. Apply pressure in the direction opposite to shoulder abduction, ensuring a gradual increase in resistance to assess the muscle's strength throughout the range of motion.
- Observation: Observe the patient's ability to maintain the position against resistance. Look for compensatory movements or substitutions, such as trunk leaning or scapular elevation, which may indicate weakness in the targeted muscle or muscles.
- Grading: Use a standardized grading scale, such as the Medical Research Council (MRC) scale or the Modified Oxford Scale, to assign a muscle grade based on the patient's performance. Grades typically range from 0 to 5, with 0 indicating no muscle contraction and 5 representing normal strength.
Shoulder Horizontal Adduction
The primary muscle responsible for this movement is the pectoralis major, specifically its sternal portion. Additionally, other muscles, including the anterior deltoid and coracobrachialis, contribute to shoulder horizontal adduction to varying degrees.
Testing Procedure for Shoulder Horizontal Adduction: Performing manual muscle testing for shoulder horizontal adduction involves several key steps to ensure accuracy and reliability.
- Positioning: Position the patient comfortably in either a supine or seated position, with the arms relaxed at their sides.
- Stabilization: Stabilize the scapula to isolate the movement to the shoulder joint. You can achieve this by providing manual stabilization of the scapula with your non-testing hand.
- Palpation: Identify the insertion point of the pectoralis major, which is typically located on the lateral aspect of the humerus.
- Testing: Instruct the patient to bring their arm across their body in the horizontal plane, mimicking the movement of hugging oneself.
- Application of Resistance: Place one hand on the distal forearm or wrist of the patient's testing arm to provide resistance. Apply pressure in the direction opposite to shoulder horizontal adduction, ensuring a gradual increase in resistance to assess the muscle's strength throughout the range of motion.
- Observation: Observe the patient's ability to maintain the position against resistance. Look for compensatory movements or substitutions, such as trunk rotation or scapular protraction, which may indicate weakness in the targeted muscle or muscles.
- Grading: Use a standardized grading scale, such as the Medical Research Council (MRC) scale or the Modified Oxford Scale, to assign a muscle grade based on the patient's performance. Grades typically range from 0 to 5, with 0 indicating no muscle contraction and 5 representing normal strength.
Scapula Elevation
The main muscle responsible for this movement is the upper portion of the trapezius muscle, specifically the descending (or upper) fibers. Additionally, other muscles, such as the levator scapulae and the rhomboids, contribute to scapular elevation to varying degrees.
Testing Procedure Scapula Elevation: Performing manual muscle testing for scapular elevation involves several key steps to ensure accuracy and reliability.
- Positioning: Position the patient comfortably in either a seated or standing position, with the arms relaxed at their sides.
- Stabilization: Stabilize the scapula to isolate the movement to the shoulder joint. You can achieve this by providing manual stabilization of the scapula with your non-testing hand.
- Palpation: Identify the insertion point of the upper trapezius, which is typically located along the lateral aspect of the superior border of the scapula.
- Testing: Instruct the patient to lift their shoulder blade upward, as if shrugging their shoulders.
- Application of Resistance: Place one hand on the distal portion of the shoulder or the upper arm of the patient's testing side to provide resistance. Apply pressure in the direction opposite to scapular elevation, ensuring a gradual increase in resistance to assess the muscle's strength throughout the range of motion.
- Observation: Observe the patient's ability to maintain the position against resistance. Look for compensatory movements or substitutions, such as trunk leaning or scapular retraction, which may indicate weakness in the targeted muscle or muscles.
- Grading: Use a standardized grading scale, such as the Medical Research Council (MRC) scale or the Modified Oxford Scale, to assign a muscle grade based on the patient's performance. Grades typically range from 0 to 5, with 0 indicating no muscle contraction and 5 representing normal strength.
Scapula Retraction and Adduction
the middle and lower fibers of the trapezius are the primary muscles responsible for this movement, as we as the rhomboid major and rhomboid minor. Additionally, other muscles, such as the serratus anterior and the posterior deltoid, play supporting roles in scapular stability and movement.
Testing Procedure for Scapula Retraction and Adduction: Performing manual muscle testing for scapular retraction and adduction involves several key steps to ensure accuracy and reliability.
- Positioning: Position the patient comfortably in either a seated or standing position, with the arms relaxed at their sides.
- Stabilization: Stabilize the scapula to isolate the movement to the shoulder joint. You can achieve this by providing manual stabilization of the scapula with your non-testing hand.
- Palpation: Identify the insertion points of the muscles involved, including the medial border of the scapula for the rhomboids and the superior border of the scapula for the middle and lower fibers of the trapezius.
- Testing Scapular Retraction: Instruct the patient to pull their shoulder blades together, as if squeezing them toward the spine.
- Application of Resistance for Retraction: Place one hand on the medial aspect of the patient's scapula or the forearm of the testing arm to provide resistance. Apply pressure in the direction opposite to scapular retraction, ensuring a gradual increase in resistance to assess the muscle's strength throughout the range of motion.
- Testing Scapular Adduction: Instruct the patient to bring their shoulder blades toward the midline of their body, as if squeezing them together.
- Application of Resistance for Adduction: Place one hand on the lateral aspect of the patient's scapula or the forearm of the testing arm to provide resistance. Apply pressure in the direction opposite to scapular adduction, ensuring a gradual increase in resistance to assess the muscle's strength throughout the range of motion.
- Observation: Observe the patient's ability to maintain the position against resistance. Look for compensatory movements or substitutions, such as shoulder shrugging or trunk rotation, which may indicate weakness in the targeted muscle or muscles.
- Grading: Use a standardized grading scale, such as the Medical Research Council (MRC) scale or the Modified Oxford Scale, to assign a muscle grade based on the patient's performance. Grades typically range from 0 to 5, with 0 indicating no muscle contraction and 5 representing normal strength.
Elbow Flexion
The primary muscle responsible for this movement is the biceps brachii, located on the front of the upper arm. Additionally, the brachialis muscle, situated beneath the biceps, also contributes significantly to elbow flexion.
Testing Procedure for Elbow Flexion: Performing manual muscle testing for elbow flexion involves several key steps to ensure accuracy and reliability.
- Positioning: Position the patient comfortably in either a seated or supine position, with the elbow fully extended and the forearm in a neutral position (neither pronated nor supinated).
- Stabilization: Stabilize the upper arm to isolate the movement to the elbow joint. You can achieve this by providing manual stabilization of the upper arm with your non-testing hand.
- Palpation: Identify the insertion point of the biceps brachii, which is typically located on the radial tuberosity of the forearm. Additionally, palpate the brachialis muscle, which lies deep to the biceps along the anterior aspect of the arm.
- Testing: Instruct the patient to flex their elbow, bringing their hand toward their shoulder while keeping the upper arm stationary.
- Application of Resistance: Place one hand on the distal forearm or wrist of the patient's testing arm to provide resistance. Apply pressure in the direction opposite to elbow flexion, ensuring a gradual increase in resistance to assess the muscle's strength throughout the range of motion.
- Observation: Observe the patient's ability to maintain the position against resistance. Look for compensatory movements or substitutions, such as shoulder shrugging or trunk leaning, which may indicate weakness in the targeted muscle or muscles.
- Grading: Use a standardized grading scale, such as the Medical Research Council (MRC) scale or the Modified Oxford Scale, to assign a muscle grade based on the patient's performance. Grades typically range from 0 to 5, with 0 indicating no muscle contraction and 5 representing normal strength.
Elbow Extension
The main muscle responsible for this movement is the triceps brachii, which consists of three heads: the long head, the lateral head, and the medial head. Additionally, other muscles, such as the anconeus, also contribute to elbow extension to varying degrees.
Testing Procedure Elbow Extension: Performing manual muscle testing for elbow extension involves several key steps to ensure accuracy and reliability.
- Positioning: Position the patient comfortably in either a seated or supine position, with the elbow fully extended and the forearm in a neutral position (neither pronated nor supinated).
- Stabilization: Stabilize the upper arm to isolate the movement to the elbow joint. You can achieve this by providing manual stabilization of the upper arm with your non-testing hand.
- Palpation: Identify the insertion point of the triceps brachii, which is typically located on the olecranon process of the ulna.
- Testing: Instruct the patient to straighten their elbow, pushing their hand downward as if trying to straighten their arm completely.
- Application of Resistance: Place one hand on the distal forearm or wrist of the patient's testing arm to provide resistance. Apply pressure in the direction opposite to elbow extension, ensuring a gradual increase in resistance to assess the muscle's strength throughout the range of motion.
- Observation: Observe the patient's ability to maintain the position against resistance. Look for compensatory movements or substitutions, such as shoulder shrugging or wrist flexion, which may indicate weakness in the targeted muscle or muscles.
- Grading: Use a standardized grading scale, such as the Medical Research Council (MRC) scale or the Modified Oxford Scale, to assign a muscle grade based on the patient's performance. Grades typically range from 0 to 5, with 0 indicating no muscle contraction and 5 representing normal strength.
Wrist Flexion
The wrist flexors, which include the flexor carpi radialis, flexor carpi ulnaris, and palmaris longus are the primary muscles responsible for this movement. hese muscles originate from the forearm and insert into the hand, allowing for the flexion of the wrist joint.
Testing Procedure for Wrist Flexion: Performing manual muscle testing for wrist flexion involves several key steps to ensure accuracy and reliability.
- Positioning: Position the patient comfortably in a seated position with the forearm resting on a stable surface, such as a table or armrest, and the wrist in a neutral position (neither flexed nor extended).
- Stabilization: Stabilize the forearm to isolate the movement to the wrist joint. You can achieve this by providing manual stabilization of the forearm with your non-testing hand or by asking the patient to grasp the edge of the table with their non-testing hand.
- Palpation: Identify the muscles involved in wrist flexion by palpating the flexor tendons along the anterior aspect of the forearm. The flexor carpi radialis is located on the radial side of the forearm, while the flexor carpi ulnaris is located on the ulnar side. The palmaris longus, if present, is located in the middle of the forearm.
- Testing: Instruct the patient to flex their wrist downward, bringing the palm of their hand closer to the underside of the forearm.
- Application of Resistance: Place one hand on the dorsum (back) of the patient's hand to provide resistance. Apply pressure in the direction opposite to wrist flexion, ensuring a gradual increase in resistance to assess the muscle's strength throughout the range of motion.
- Observation: Observe the patient's ability to maintain the position against resistance. Look for compensatory movements or substitutions, such as finger flexion or forearm rotation, which may indicate weakness in the targeted muscle or muscles.
- Grading: Use a standardized grading scale, such as the Medical Research Council (MRC) scale or the Modified Oxford Scale, to assign a muscle grade based on the patient's performance. Grades typically range from 0 to 5, with 0 indicating no muscle contraction and 5 representing normal strength.
Wrist Extension
The primary muscles responsible for this movement are the wrist extensors, which include the extensor carpi radialis longus, extensor carpi radialis brevis, extensor carpi ulnaris, and extensor digitorum communis. These muscles originate from the forearm and insert into the hand, allowing for the extension of the wrist joint.
Testing Procedure for Wrist Extension: Performing manual muscle testing for wrist extension involves several key steps to ensure accuracy and reliability.
- Positioning: Position the patient comfortably in a seated position with the forearm resting on a stable surface, such as a table or armrest, and the wrist in a neutral position (neither flexed nor extended).
- Stabilization: Stabilize the forearm to isolate the movement to the wrist joint. You can achieve this by providing manual stabilization of the forearm with your non-testing hand or by asking the patient to grasp the edge of the table with their non-testing hand.
- Palpation: Identify the muscles involved in wrist extension by palpating the extensor tendons along the posterior aspect of the forearm. The extensor carpi radialis longus and brevis are located on the radial side of the forearm, while the extensor carpi ulnaris is located on the ulnar side. The extensor digitorum communis runs centrally along the forearm.
- Testing: Instruct the patient to extend their wrist upward, bringing the back of their hand closer to the underside of the forearm.
- Application of Resistance: Place one hand on the palm of the patient's hand to provide resistance. Apply pressure in the direction opposite to wrist extension, ensuring a gradual increase in resistance to assess the muscle's strength throughout the range of motion.
- Observation: Observe the patient's ability to maintain the position against resistance. Look for compensatory movements or substitutions, such as finger flexion or forearm rotation, which may indicate weakness in the targeted muscle or muscles.
- Grading: Use a standardized grading scale, such as the Medical Research Council (MRC) scale or the Modified Oxford Scale, to assign a muscle grade based on the patient's performance. Grades typically range from 0 to 5, with 0 indicating no muscle contraction and 5 representing normal strength.
Following these ten upper extremity manual muscle testing steps is a valuable assessment tool in physical therapy practices, providing insights into muscle strength and function. By following standardized procedures and best practices, clinicians can accurately evaluate the upper extremities of the body across major muscle groups. This aids in the development of targeted rehabilitation plans and tracking patient progress effectively.
For more in-depth information on manual muscle tests please visit the following website: https://www.physio-pedia.com/Muscle_Strength_Testing
Related Blog Posts:
A Guide to Mastering Lower Extremity Manual Muscle Testing with Handheld Dynamometers
Is Manual Muscle Testing Really Objective?
Handheld Dynamometers for sell:
Handheld Dynamometers for Manual Muscle Testing
Recent Posts
-
Understanding Carpal Tunnel Syndrome: Prevention and Treatment
Carpal Tunnel Syndrome (CTS) is a prevalent and often debilitating condition affecting millions of i …May 9th 2024 -
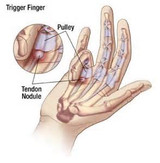
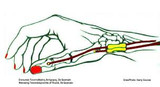
Trigger Finger Prevention and Treatment
Trigger Finger, medically known as stenosing tenosynovitis, is a condition that affects the fingers, …May 8th 2024 -
Understanding De Quervain’s Tenosynovitis: Prevention and Treatment Strategies
De Quervain’s Tenosynovitis, though lesser-known than some other wrist conditions, can cause signifi …May 7th 2024